Author- Dr. Md. Shamim, MD.
Introduction of Diabetic Ketoacidosis:
Diabetic ketoacidosis is a disorder mainly in patient with type 1 Diabetes Mellitus, but may occur in Type 2 Diabetes Mellitus also. It may result from increased insulin requirements in Type 1 Diabetes mellitus during infection, trauma, Myocardial Infarction, or surgery. It is a life-threatening medical emergency with mortality rate <5% individual under 40 years of age, but more severe prognosis in older people with mortality rate >20%.
Essential criteria for diagnosis of Diabetic Ketoacidosis:
- Hyperglycaemia (Blood glucose level >250 mg/dl).
- Metabolic acidosis- blood pH <7.3 & serum HCO3– <15 mg/L.
- Ketone bodies +ve in serum.
Therapeutic Goal of Diabetic Ketoacidosis:
- To restore plasma volume.
- To reduce blood glucose level and osmolality.
- To correct acidosis.
- To replenish electrolyte losses.
- To identify and treat precipitating factors.
Treatment of Diabetic Ketoacidosis:
- Admit in ICU
- A- Maintain patency of airway
- B- Breathing, spO2 >90%. Intubation and mechanical ventilation
- C- Circulation, IV-line access
- D- Drugs (Insulin)
- E- Electrolytes replacement
- F– Fluid replacement.
Fluid replacement
- Fluid deficit 4 to 5 L.
- Fluid of choice 0.9% NS.
- Should be started in emergency department as soon as diagnosis is established
- Should be infused @ 1 L/hour over the first 1 to 2 hour.
- After the first 2 L of fluid have been given, IV fluid infusion should be @ 300 to 400 ml/hour.
- Use 0.9% NS unless the serum sodium is >150mEq/L, then 0.45% of NS should be used.
- The volume status should be monitor Clinically.
- If volume replacement < 3 to 4 L in 8 hours, difficult to restore normal perfusion.
- If volume replacement > 5 litre in 8 hours, Acute Respiratory Distress Syndrome (ARDS) and cerebral oedema may occur.
- When blood glucose levels fall to Approx. 250 mg/dl, the fluid should be changed to 5% glucose containing solution to maintain serum glucose in the range of 250 to 300 mg/dl. This will prevent development of hypoglycaemia and cerebral oedema due to rapid decline of blood glucose level.
Insulin replacement
- Immediately after initiation of fluid replacement.
- Type of insulin- HIR
- Loading dose- 0.1 Unit/Kg IV bolus prime the tissue insulin receptors
- Followed by 0.1 Unit/kg/hour continuously IV infused to replace the deficit of insulin.
- If blood glucose level fails to fall at least 10% in the first hour, repeat loading those (0.1 unit per kg) recommended.
The insulin dose should be adjusted to lower the blood glucose level by about 50 to 70 mg/dl/hour.
Potassium
Total body potassium loss from polyuria and vomiting may be as high as 200mEq.
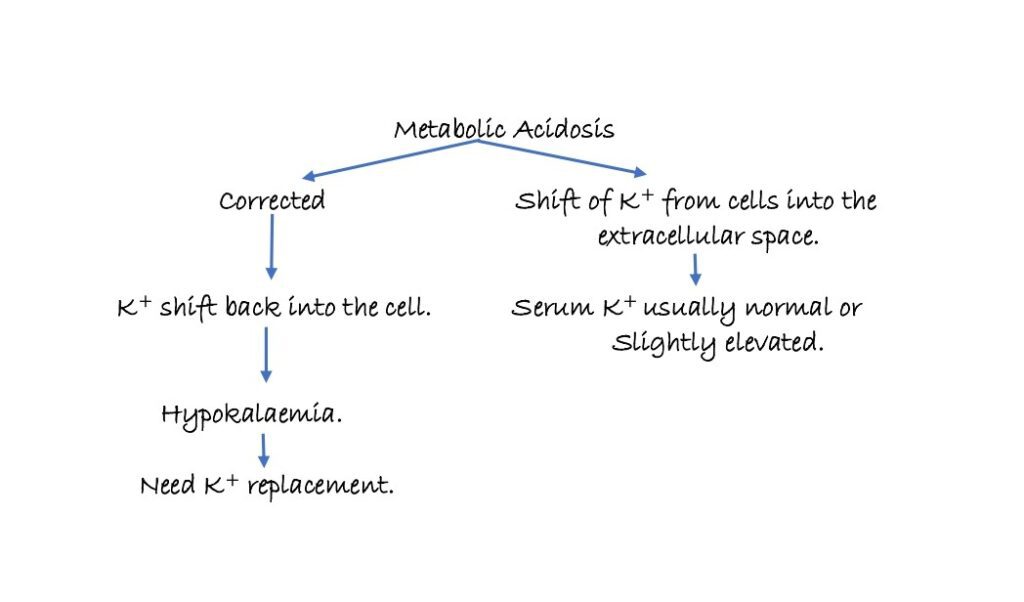
- Potassium replacement should be started as soon as metabolic acidosis starts to resolve.
- Potassium Chloride (KCl)- 10 to 30mEq/hour should be infused during 2nd and 3rd hours after beginning of therapy.
- Food high in potassium content should be prescribed when the patient has recovered sufficiently to take food orally.
- Tomato juice has 14mEq of K+/240 ml, and a medium sized banana contains about 10mEq of potassium.
Sodium Bicarbonate (NaHCO3–)
- The use of sodium bicarbonate in the management of DKA has been questioned because of the following potentially harmful consequences:
- Development of hypokalaemia from rapid shift of K+ into the cells due to overcorrected metabolic acidosis.
- Tissue anoxia from reduced dissociation of oxygen from haemoglobin when metabolic acidosis is rapidly reversed.
- Cerebral acidosis resulting from lowering of CSF pH.
Therefore, it is recommended that HCO3– should be administered in DKA, if the arterial blood pH is ≤ 7.0
One or two ampoules of NaHCO3– (1 ampoule contains 44mEq/50ml) should be added to 1 L of 0.45% saline with 20mEq KCl and infused over 1 to 2
hour.
Phosphate
- Phosphate requirement is seldom required in treating DKA.
- However, if severe hypophosphatemia of less than 1mEq/dl develops during insulin therapy, or small amount of phosphate can be replaced per hour as the potassium salt.
Hyperchloremic acidosis during therapy
- A portion of the bicarbonate deficit is the placed with chloride ions infused in large amounts as NS to correct the dehydration.
- Plasma lyte solution (pH- 7.4, Cl– 98mEq/L) instead of NS (pH- 5.5, Cl- 154mEq/L) should be used to prevent hyperchloremic acidosis.
Treatment of associated infections
- Antibiotics should be prescribed as causative organisms identified.
Transition to subcutaneous Insulin regimen
- Once the DKA is controlled and the patient is awake and able to eat, subcutaneous insulin therapy can be initiated.
References:
- CMDT.
- Harrison’s Principle of Internal Medicine.
- Katzung, Basic & Clinical Pharmacology.
- Adult Diabetic Ketoacidosis
- Diabetic Ketoacidosis
